We are excited to announce that future pearls will be posted on the Academic Life in Emergency Medicine site. Pearls previously posted here will stay active and we will continue to post other original content!
Updated Gonorrhea Treatment Recommendations from CDC
Today’s pearl summarizes the recent updates from the CDC’s Treatment Guidelines for Gonococcal Infection.
Which antibiotics and what doses should be used? How do we reach effective concentrations in all patients?
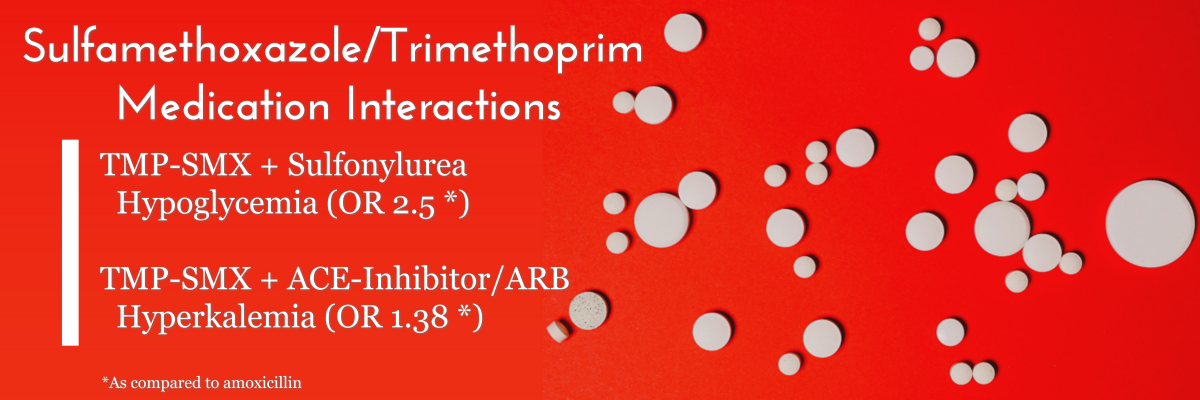
Continue reading “Updated Gonorrhea Treatment Recommendations from CDC”Sulfamethoxazole/Trimethoprim Drug Interactions Important for EM Clinicians
Today’s pearl highlights two interactions that are important for Emergency Medicine clinicians to know.
What are the risks? How common are they?
Continue reading “Sulfamethoxazole/Trimethoprim Drug Interactions Important for EM Clinicians”Antibiotic Effects on Oral Contraceptives
Today’s pearl addresses a misconception regarding a drug interaction between oral contraceptives and antibiotics.
Are back-up methods of contraception required? Does this apply to all antibiotics?
Continue reading “Antibiotic Effects on Oral Contraceptives”Neuropsychiatric Side Effects of Steroids
Today’s pearl reviews the adverse neuropsychiatric effects associated with the use of steroids.
Can steroids alter mentation? What is the incidence? Are there any risk factors?
Continue reading “Neuropsychiatric Side Effects of Steroids”Beta-Agonist Alternatives to Nebulized Albuterol for Treatment of Hyperkalemia
Today’s pearl provides some alternative methods to treat patients with hyperkalemia if nebulized albuterol is not an option.
What route? Which medication? How much?
Continue reading “Beta-Agonist Alternatives to Nebulized Albuterol for Treatment of Hyperkalemia”Magnesium for Atrial Fibrillation Rate Control in the ED
Today’s pearl is a continuation of Pearl 42: Medication Pearls for Atrial Fibrillation Management in the ED and reviews the role of magnesium for the treatment of atrial fibrillation.
Does magnesium reduce HR? How much and how fast to administer?
Continue reading “Magnesium for Atrial Fibrillation Rate Control in the ED”Medication Pearls for Atrial Fibrillation Management in the ED
Today’s pearl highlights 5 main points related to the treatment of atrial fibrillation.
Should you give a beta blocker or a calcium channel blocker? What dose should you use?
Continue reading “Medication Pearls for Atrial Fibrillation Management in the ED”QTc Prolongation and Torsades de Pointes with Droperidol in the Emergency Department
How common is QTc prolongation or Torsades de Pointes (TdP) in ED patients getting droperidol?
Actually quite rare!
In 30,000 patients, TdP occurred once (the patient had multiple risk factors and TdP didn’t reoccur when re-challenged).
Prior data covered in 2015 @aaeminfo position statement.